Do you experience Fatigue, GI discomfort, Food intolerances, Poor sleep, Headaches, or Pain & inflammation?
Do you long for more energy, less pain, and a happy gut?
If you answered yes to any of these, join us for a guest speaker, Metagenics Rep Becky Cortez, as she discusses her Core 4 supplements to combat these issues. Monday, October 22nd 1pm at 18153 Club View Drive. Please RSVP!
We will get to know Metagenics Manufacturing Quality and how Metagenics actively goes beyond what’s required!
If you missed this talk, here are the Core 4 vitamins that Becky discussed:
CORE 4
by Ashley Jordan Ferira, PhD, RDN
If you can have a favorite nutrient, mine would be vitamin D. Unlike other nutrients, this fat-soluble vitamin is obtainable via several unique routes: the skin with adequate UVB exposure, a handful of natural food sources, a few fortified foods, dietary supplements, and even prescription drugs.
Whether consuming vitamin D2 or D3 (FYI, the latter more potently impacts vitamin D status),1 vitamin D ultimately circulates in the 25-hydroxyvitamin D [25(OH)D] form (the clinical biomarker used to measure vitamin D status) and acts throughout the body as a pleiotropic hormone in its active form, 1,25-dihydroxyvitamin D [1,25(OH)2D].
Historically famous for its essential, classical role in calcium and phosphorus homeostasis and bone physiology (think rickets prevention), the past few decades of research have unveiled diverse, extraskeletal health roles for vitamin D, including but not limited to the immune system, cardiometabolic pathophysiology, cancer, pregnancy, etc.
Few foods naturally contain vitamin D (e.g., egg yolk, certain fatty fish, fish liver oil, and certain species of UV-irradiated mushrooms), and fortified foods offer relatively small amounts (e.g., 100 IU vitamin D per 8 oz cup of fortified milk or orange juice),2 so vitamin D supplementation becomes a strategic solution. In the eloquent words of pediatrician and vitamin D researcher, Carol Wagner, MD: “Something so simple- vitamin D supplementation- could improve the health status of millions and so becomes an elegant solution to many of our health problems today.”
If it’s possible to be defensive of a micronutrient, I am protective of vitamin D. Non-evidence-based rumors and negative media attention targeting vitamin D are common. Some of the misinformation is hype from anti-supplement camps who make broad, sweeping statements that lack scientific substantiation. But not all of the vitamin D myths originate from bias or lack of intellectual rigor. After all, who has time to keep up with the impressive, daily output of new vitamin D research? Clinicians certainly do not have the luxury of time, not in the current healthcare paradigm. Nevertheless, when inaccurate conclusions are propagated to patients about vitamin D and their health, that’s more harm than good. So, let me help out.
This blog series explores some of the most common vitamin D myths. Let’s tackle just 1 myth today:
Myth: I get enough vitamin D from food, so I don’t need a vitamin D supplement.
Can you meet your vitamin D needs from food alone? Well, that depends on how you define “needs.” Let’s talk about the 2 major (and quite different) sets of vitamin D recommendations.
First, the National Academy of Medicine (NAM), formerly known as the Institute of Medicine, provided vitamin D Recommended Dietary Allowances (RDAs) in 2010.3 Here’s how much vitamin D NAM says that we (Americans and Canadians) need based on bone health research (think rickets and osteomalacia prevention, calcium absorption, etc.):3
- Infants (0-1 year): 400 IU/day
- Children and Adults (1-70 years): 600 IU/day
- Older Adults (71+ years): 800 IU/day
But I have a bone to pick (pun intended) with NAM’s vitamin D recommendations. I find them to be problematic, if not contradictory at times, for a few key reasons.
To start with, the RDA is by definition “the average daily level of intake sufficient to meet the nutrient requirements of nearly all (97-98%) healthy people.”4 Well, that misses the unhealthy people. Since 2/3rd of the country are overweight or obese5 and heart disease and cancer are the #1 and #2 causes of mortality in the US, respectively,6 one can extrapolate that the vitamin D RDAs do not apply to a decent chunk of the gen pop.
In fact, research indicates that overweight and obese individuals require more vitamin D than their lean counterparts,7 but the NAM recommendations fail to consider adiposity.
Second, lumping a toddler and 68-year-old grandmother in the same RDA category (i.e., ages 1-70 years) seems to lack nuance. Skeletal health is critical throughout life, but you cannot tell me that the vitamin D needs for the rapidly accruing skeleton in childhood and adolescence are no different than an adult or older adult’s skeletal needs.
Third, the RDAs for daily vitamin D intake are incongruent with the serum 25(OH)D cutoffs NAM also published in 2010. They provided the following 25(OH)D categories:
- Deficiency: ≤ 12 ng/mL
- Insufficiency: 12-19 ng/mL
- Sufficiency: ≥ 20 ng/mL
The problem is that the vitamin D RDAs won’t get you into the 25(OH)D range for sufficiency. UVB sun exposure can except cutaneous vitamin D synthesis from sun is highly variable and limited for many, but 400-800 IU/day of vitamin D simply won’t do the trick. It’s like asking someone to fill up an aquarium tank with water and giving them a few cups of water to do the trick. In the sage words of the late Bob Heaney, MD: “We’ve been able to show that the (vitamin D) RDA barely budges the blood 25-hydroxyvitamin D level.”8
Thanks to Dr. Heaney, who made invaluable research contributions to the field of vitamin D, we know that 100 IU/day of vitamin D increases serum 25(OH)D concentrations by approximately 1 ng/mL.9 That means that 1,000 IU/day of vitamin D would raise 25(OH)D by about 10 ng/mL. Although weight status, age, and the patient’s baseline vitamin D status can variably impact the supplementation response, this “rule of thumb” can be used to roughly calculate vitamin D supplementation needs.
For example, let’s take a patient: me. I have limited UVB sun exposure and consume some foods that contain vitamin D (e.g., milk, eggs, salmon) but irregularly. My daily 5,000 IU vitamin D3 supplement has my serum 25(OH)D at 54 ng/mL. It stays between 50-60 ng/mL, which is in the sufficient range.
But I’m an anomaly. Nationally representative research backs up the fact that Americans are not getting adequate vitamin D from their diets.10-11 First, 93% of Americans 2 years and older are failing to consume at least 400 IU/day of vitamin D from diet alone, and this estimate includes fortified food sources.10 Even when diet plus sun exposure are both thrown into the mix, about 1/3rd of the US population has serum 25(OH)D levels associated with vitamin D insufficiency or deficiency.11 For more details on vitamin D deficiency and why it persists, check out this blog.
Dietitians (I am one) and other clinicians love to preach “food first.” That slogan is true but ignores research on key nutrient gaps. I prefer to say, “food first, then fill the gaps.” And in the case of vitamin D, the gap is practically guaranteed, except for the outlier patient who’s knocking back fish liver oils and irradiated mushrooms.
Lastly, a more current and scientifically and clinically nuanced set of guidelines exist. One year after the NAM recommendations were released, several of the world’s leading vitamin D researchers convened to review the evidence to date, resulting in the 2011 publication: Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline.12
The US Endocrine Society’s conclusions are harmonious with the mindset of a clinician, who is tasked with addressing the vitamin D needs of unique patients. The guideline recommends higher daily vitamin D levels than NAM, with a different and logical purpose in mind: Raising serum 25(OH)D levels into the sufficient range (≥ 30 ng/ml):12
- Infants (0-1 year): At least 1,000 IU/day
- Children and Adolescents (1-18 years): At least 1,000 IU/day
- Adults (19+ years): At least 1,500 – 2,000 IU/day
The US Endocrine Society also provided the following 25(OH)D cutoffs:12
- Deficiency: ≤ 20 ng/mL
- Insufficiency: 21-29 ng/mL
- Sufficiency: ≥ 30 ng/mL
The guidelines even differentiate vitamin D needs based on adiposity: Children and adults who are obese may need 2-3 times more vitamin D daily than normal-weight individuals.12 Finally, the US Endocrine Society provides clear guidance for correcting vitamin D deficiency in all age groups, with repletion and maintenance dosing information, which is a topic that I will cover in a future blog.
Individual genetic differences for the vitamin D receptor (VDR) (i.e., gene polymorphisms like Cdx2, Apa1, Fok1, Taq1) are another important facet to weave into each patient’s unique vitamin D story, underscoring the prudence of a personalized lifestyle medicine approach to treat the individual.
Takeaway:
No, you cannot satisfy your vitamin D needs from food alone. If you plan to raise and maintain your serum 25(OH)D level (the biomarker that indicates vitamin D status) in the sufficient range for skeletal and extraskeletal health, that will require daily vitamin D supplementation. Remember, 30 ng/mL is not the goal. It’s the cutoff for insufficiency.
Here’s a peak at some of the additional vitamin D myths that will be covered in future blogs:
- It doesn’t matter what kind of vitamin D form you consume in food or supplements; vitamin D2 and D3 are the same.
- Vitamin D is a fat-soluble vitamin, so it’s toxic when you take too much!
- Vitamin D supplements are hype, unregulated, and lacking sound science to back up their clinical use and recommendation.
- After my patient is replete in vitamin D, maintenance dosing is not needed.
Do you have a question about the science and clinical application for vitamin D? Let me know by commenting below!
2. Probiotic
by Melissa Blake, BSc, ND
The use of probiotics has grown substantially over the last several years. Propelled by development in sequencing methods and analytical techniques, there has been a significant increase in knowledge and understanding about the importance of a healthy microbiome.1
The currently accepted definition of a probiotic states they are “live microorganisms which when administered in adequate amounts confer a health benefit on the host”.2 Is this relatively broad definition sufficient for clinicians to guide treatment? Can we assume that any live organism in relevant doses will achieve positive clinical outcomes? We’ve been talking about the use of probiotics for over a hundred years,6 but when it comes to probiotic therapy, what do we really know?
The human microbiome
A balanced and diverse microbiota plays a role in human health during the lifecycle. Growing evidence supports a connection between maternal microbiome and pregnancy outcomes, including preterm birth, preeclampsia, gestational hypertension, and gestational weight gain, as well as having an impact on infant health.10
Infancy is a critical time in the development of commensal gut bacteria and is influenced by pre- and postnatal exposures, including the maternal microbiome, delivery method (C-section vs. vaginal birth), diet, and medical interventions.11 Such factors can negatively or positively influence the balance of an individual’s microbiome and may impact short- and long-term health outcomes.12
Modifications to the infant gut microbiota may impact childhood obesity risk,13 atopic disease,14 as well as various GI conditions.15 After initial colonization, factors such as age, gender, diet, environment, stress, and the use of antibiotics continue to influence the microbiome.
Changes in the GI and respiratory microbiome of adults have been implicated in the pathogenesis of chronic pulmonary diseases, including asthma and allergies.16 Dysbiosis has also been associated with psoriasis,17-18 psoriatic arthritis,18 and inflammatory bowel disease,19 suggesting a direct link between a balanced microbiome and the health of the GI and immune systems. Studies have also connected highly abundant levels of specific genera of bacteria with leanness and have shown they play a role in regulating blood sugar and insulin levels.20
Recent reports suggest that neuroinflammation is an important causal mechanism in cognitive decline. This inflammatory status could be triggered by changes in the gut microbiota composition.21 Evidence is connecting the dots between gut bacteria, altered intestinal permeability, and blood brain barrier integrity.22 A disruption in gut flora may, through several mechanisms, contribute to a “leaky brain”, making the brain more susceptible to circulating substances and contributing to cognitive dysfunction. Further research is warranted in this exciting area of scientific study.
As clinicians, we cannot erase the past or possibly impact all the factors that influence the microbiome of our patients. However, we can partner with our patients to help them make positive lifestyle changes. Diet and targeted probiotic therapy are powerful tools. Consumption of excess saturated fats and added sugar influences the microbiota composition, which may lead to an imbalanced microbial population in the gut.22 By modifying risk factors and targeting the microbiome, Functional Medicine practitioners have an opportunity to both prevent and manage disease with individualized nutrition and probiotic therapy at any age.
3. Omega 3
by Ashley Jordan Ferira, PhD, RDN
You may have heard that many Americans are not getting enough vitamin D, calcium, potassium, etc. from their diet. But do you think about omega-3s as a nutrient gap? You should. Findings from the National Health and Nutrition Examination Survey (NHANES) demonstrate that > 90% of Americans are not meeting recommendations for omega-3 intake, with key differences observed in age, sex, and ethnicity subgroups.1
Although the cardiovascular benefits of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) have been demonstrated in observational and interventional studies,2-3 recent research reveals that the majority of the US population is not meeting recommended levels for fish or omega-3 fatty acid intake.4 Aside from purified omega-3 supplements, the richest dietary source of EPA and DHA is oily fish, including salmon, mackerel, herring, lake trout, sardines, and albacore tuna.5
The American Heart Association (AHA) recommends:2
- Heathy individuals: consume a variety of oily fish at least 2 servings per week, which provides about 500 mg/day of EPA + DHA
- Patients with coronary heart disease (CHD): 1 g/day of combined EPA + DHA, from oily fish and/or fish oil supplementation in consultation with a physician
- Patients needing triglyceride-lowering: 2 – 4 g/day of supplemental EPA + DHA under physician’s care
The present study investigated the long-chain omega-3 intake (EPA and DHA) across key age, sex, and ethnicity subgroups in the US.1 NHANES 2003-2008 data for 24,621 individuals was used, capturing EPA and DHA intake from both foods and supplements.
Study findings for long-chain omega-3 intake:
- Over 90% of the US population consumed < 500 mg/day of EPA+DHA from food
- Median intake from food was only 110 mg/day
- For the top consumers, fish was the #1 dietary contributor
- Men ≥ 20 years old had the highest intake
- Children, women of childbearing age, pregnant women, and lactating women had the lowest intake
- Mexican-Americans were the ethnicity with the lowest intake
- Only 6.2% reported omega-3 supplement use, which did not significantly alter the median daily intake from food
Why is this Clinically Relevant?
- EPA and DHA are heart-healthy, long-chain omega-3 fatty acids that are one of the most prevalent nutrient gaps in the US
- Children, women of childbearing age, pregnant/lactating women, and Mexican Americans are subgroups consuming the lowest levels of EPA and DHA
- Through targeted dietary and supplement recommendations, clinicians can help patients address their omega-3 “gap” and meet AHA guidelines
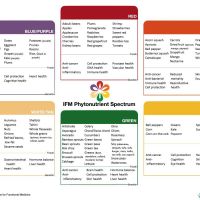
4. Phytomulti
Taken From Metagenics Institute:
You try to eat well to feel good and stay healthy. While it’s optimal to get your daily nutritional needs from the foods you eat, it’s just plain difficult. There is conflicting information out there on the benefits of supplements, but the Dietary Guidelines for Americans 2015-2020 say that supplements may be useful for providing the nutrients you may be lacking from diet alone.
Still on the fence? Consider these top five reasons to add a multivitamin to your daily regimen.
1. Healthy aging. As we get older, our bodies have a harder time absorbing nutrients from food. The National Institute on Aging notes that starting around age 50, people begin to require increased amounts of certain vitamins and minerals.1,2 In fact, according to a study published in the American Journal of Clinical Nutrition, researchers found that taking a daily multivitamin & mineral supplement may help improve micronutrient deficiencies associated with aging.3
2. Making up for eliminated food groups. While some people have to cut certain foods like nuts or gluten out of their diets due to allergies, many eliminate particular foods or food groups from their diet voluntarily. This can cause vitamin insufficiencies and deficiencies that would be helped with a multivitamin. Trying a paleo diet? You might risk a shortage of calcium or vitamin D by eliminating dairy or grains. Cutting back on red meat? A multivitamin will replace the iron and B12 you would normally get from diet.
3. Getting the RDAs you’re not getting from food. You’ve probably heard that the typical Western diet doesn’t include nearly enough fruits, vegetables, whole grains, legumes, or lean protein. Because of that, you don’t always reap the vitamin and mineral benefits that those foods naturally supply. Consequently, nationally US adults are routinely failing to meet their daily requirements for vitamin A, C, D, E, and K, as well as for calcium, magnesium and potassium from diet alone, and this is including fortified sources!4Supplementing with a multivitamin is therefore a prudent way to strategically fill those gaps on a daily basis. After all, the goal should not simply be to avoid blatant vitamin deficiencies, like scurvy with vitamin C deficiency. Borderline vitamin and mineral insufficiencies are just as important to avoid and address. Even the most health-conscious eater will benefit from multivitamin support to achieve micronutrient sufficiency across the board.
4. Getting that extra energy to get through the day. In today’s “go-go-go” society, one of the top complaints is a general lack of energy. Instead of reaching for that third cup of coffee, remember that your cells require certain vitamins and minerals to power your busy life; especially if you’re not getting a full eight hours of sleep or eating a balanced diet, a multivitamin can help provide the nutrients you need to feel energetic throughout the day.5
5. Managing stress. Daily life stressing you out? You’re not alone. But vitamins and minerals play significant biochemical roles in supporting and preserving your brain’s cognitive processes, and studies have shown that a daily multivitamin—particularly one with high doses of B vitamins—can help to reduce stress and support a healthy mood.6
Ready to add a daily multivitamin to your diet? Be sure to check with your healthcare practitioner to see if he or she has personalized recommendations for you and to ensure that any medications you’re currently on won’t interfere with their effectiveness or the effectiveness of the multivitamin ingredients.
My favorite Multi. I like to buy the larger size and order on Auto so I never run out!
Do you experience Fatigue, GI discomfort, Food intolerances, Poor sleep, Headaches, or Pain & inflammation?
Do you long for more energy, less pain, and a happy gut?
If you answered yes to any of these, join us for a guest speaker, Metagenics Rep Becky Cortez, as she discusses her Core 4 supplements to combat these issues. Monday, October 22nd 1pm at 18153 Club View Drive. Please RSVP!
We will get to know Metagenics Manufacturing Quality and how Metagenics actively goes beyond what’s required!



![met2273-ultraflora-fact-sheet[1]](https://idealnutritionblog.files.wordpress.com/2018/10/met2273-ultraflora-fact-sheet1.png?w=1086)










1 thought on “Core 4 Supplements by Becky Cortez, RD, LDN”